Introduction
Value-based healthcare is gaining popularity as an approach to increase sustainability in healthcare. It has its critics, possibly because its roots are in a health system where part of the drive for a hospital to improve outcomes is to increase market share by being the best at what you do. This is not really a solution for improving population health and does not translate well to publicly-funded healthcare systems such as the NHS. However, when we put aside dogma about how we would wish to fund healthcare, value-based healthcare provides us with a very useful set of tools with which to tackle some of the fundamental problems of sustainability in delivering high quality care.
What is value?
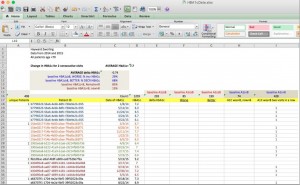
Defined by Professor Michael Porter at Harvard Business School, value is defined as a function of outcomes and costs. Therefore to achieve high value we must deliver the best possible outcomes in the most efficient way, outcomes which matter from the perspective of the individual receiving healthcare and not provider process measures or targets. Sir Muir Gray expands on the idea of technical value (outcomes/costs) to specifically describe ‘personal value’ and ‘allocative value’, encouraging us to focus also on shared decision making, individual preferences for care and ensuring that resources are allocated for maximum value.
This article seeks to demonstrate that the role of data and informatics in supporting value-based care goes much further than the collection and remote analysis of big datasets – in fact, the true benefit sits much closer to the interaction between clinician and patient.



 Data is not always the path to identifying good medicine. Quality and cost measures should not be perceived as “scores,” because the health care process is neither simplistic nor deterministic; it involves as much art and perception as science—and never is this more the case than in the first step of that process, making a diagnosis.
Data is not always the path to identifying good medicine. Quality and cost measures should not be perceived as “scores,” because the health care process is neither simplistic nor deterministic; it involves as much art and perception as science—and never is this more the case than in the first step of that process, making a diagnosis. The phrase “
The phrase “ Get a group of health policy experts together and you’ll find one area of near universal agreement: we need more transparency in healthcare. The notion behind transparency is straightforward; greater availability of data on provider performance helps consumers make better choices and motivates providers to improve. And there is
Get a group of health policy experts together and you’ll find one area of near universal agreement: we need more transparency in healthcare. The notion behind transparency is straightforward; greater availability of data on provider performance helps consumers make better choices and motivates providers to improve. And there is