By MARIE COPOULOS
I’ve had the great fortune of spending much of my career at the intersection of health care innovation and the underlying data that drives new models.
For those of us who’ve worked in this space for a long time, there’s a certain pattern recognition that comes with this work that is often immediate and obvious – both in terms of really cool developments but also gotchas. “Ah, you’re stumbling here. Everyone does that.”
The challenge, I’ve found, is that these ‘gotchas’ that can be so visible to the folx who’ve worked in health tech for the past few decades can be counterintuitive in the business and even met with resistance. Why?
I’m going to focus here on pattern recognition, with the goal of highlighting common stumbling blocks and, critically, ways you can interrupt them if you see them.
Pattern #1: Lacking a Clear-Eyed View of Market Data Gaps
Key Question: Do you understand how the market you’re in informs your ability to measure your work and use data to drive insight?
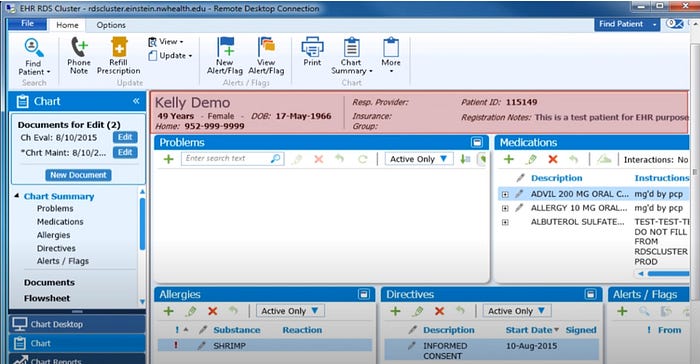
For those of you building models that change the status quo – this is for you. By nature these innovations break from existing care and financial models with the goal to improve them. We need this in health care. However, it’s common to overlook the fact that breaking with the status quo also breaks with the ways that we capture and serve up health data.
To this end, don’t assume you will be able to measure and show success, and that the data you need must be out there. The true differentiator is for both to align. Design with intention.
If you’re at the stage of thinking about a productized solution to a health care problem, then it is also the right time to look at the market with a lens toward data availability. In your problem space, what’s the data set you’re likely to lean on? Is it sufficient?
If the answer is that the data is not available or notoriously problematic in your market space for the problem you’re solving, this merits a pause. Can you find a way to survive in this reality? Can you create the data set you need? Can you adjust what you’re doing in some way to align with what is available? Is qualitative feedback ok?
Pattern #2: Accumulating Non-Technical Roadblocks Key Question: Do you have a good handle on the non-technical challenges impacting your data business?
A decade ago I would have approached this question differently. Technical challenges were often paramount as we tried to figure out how to solve the basics. Today, however, it’s often the opposite, in that business challenges are more likely to slow down technical progress than the other way around.
Continue reading…