BY ANISH KOKA
I recently saw a young man who came to see me because his place of future employment, a large health system was requiring him to complete the 1º series of his COVID-19 vaccination. He was concerned because he had chest pain after his first mRNA vaccine and was uncomfortable with the risks of a second mRNA dose. He attempted to get a Johnson and Johnson vaccine and was told by pharmacists he was not allowed to mix and match this particular vaccine as he had already received an mRNA dose. With no other option, he came to ask me whether I thought a vaccine exemption was reasonable in his case. He already had a family medicine physician sign an exemption that had been denied by his future employer’s vaccine exemption committee. The young man works on the “back end” of the health system remotely from home and he has no patient contact. The entire process has caused him to lose his health insurance from his former employer, and he was now paying out of pocket for an expensive COBRA health insurance plan. What follows is my letter to the vaccine exemption review committee regarding his case. (Published with permission, only the relevant names have been changed/redacted)

Dear Vaccine Exemption Review Committee,
I am writing this letter on behalf of John Smith DOB: xx/xx/xx in regard to a mandate from xxxx Health that Mr. Smith receive a second dose of an mRNA vaccine to complete his primary COVID-19 vaccine series.
Mr. Smith has asked me to render an opinion specifically related to his cardiac risk of receiving a second dose of an mRNA vaccine. I am a board-certified cardiologist in Philadelphia, Pennsylvania, and have been in active clinical practice for 13 years.
After reviewing the details of his case, I have grave concerns about compelling him to receive a second dose of an mRNA vaccine and would like to outline the reasons for my conclusion in this letter. I am going to specifically discuss his risk of an important, now well-recognized, adverse event: vaccine myocarditis.
What follows is some important background information about vaccine myocarditis that has been gleaned over the last 2 years before I discuss the particulars of Mr. Smith’s case.
It is relevant to note here that as a physician active clinically in both the inpatient and outpatient arenas, I am an eyewitness to the severe toll COVID-19 took on my patients in the Spring or 2020. I was impressed enough with the initial mRNA vaccine data to acquire the vaccine available from the Philadelphia Department of Health (Moderna) and ran multiple vaccine clinics in order to vaccinate my mostly high-risk patients.
What follows is data produced since the vaccine rollout that is relevant to Mr. Smith’s case.
The mRNA vaccines cause myocarditis
The risks of the novel mRNA vaccine were first clarified in April 2021 by Israeli researchers who first identified a causal link between the mRNA vaccines and myocarditis and also noted the higher incidence of myocarditis after the “second dose in young males.”
The highest incidence of vaccine myocarditis is in young men after the second dose
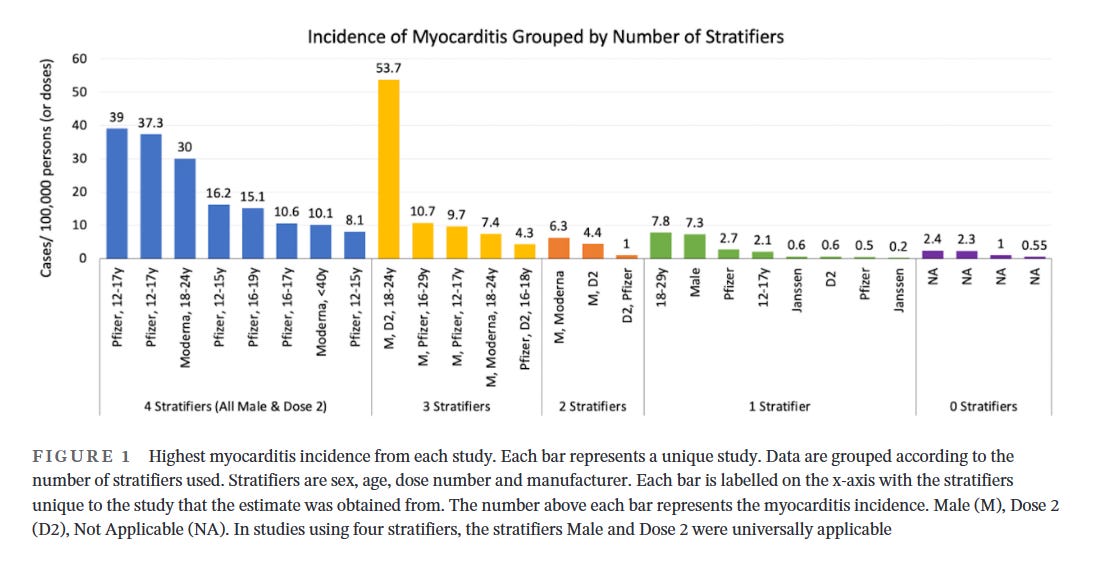
A number of subsequent studies that have attempted to quantify the risk of myocarditis are of variable quality largely because a number of studies used pooled risk estimates across the entire population, ignoring the observation that vaccine myocarditis has its highest incidence in young males. Studies that examine the incidence of myocarditis by age, sex, dose and manufacturer provide the most granularity with regard to risk estimation. A systematic review of vaccine myocarditis papers clearly demonstrates the highest incidence of vaccine myocarditis in young males after dose 2, and also highlights the uselessness of papers that do not stratify incidence of myocarditis by age, sex and dose of vaccine.
Vaccine myocarditis is higher risk than COVID myocarditis in young men
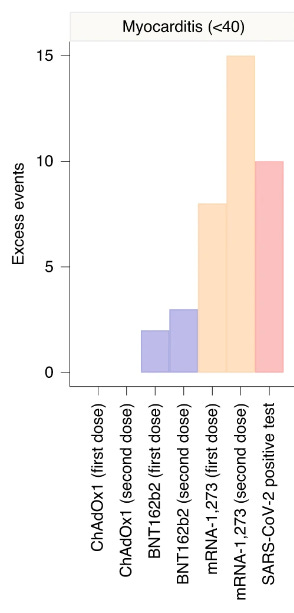
A comprehensive study from England clearly demonstrated vaccine myocarditis to be more common than COVID19 myocarditis in age < 40 despite the fact this study greatly overestimates COVID19 myocarditis rates because it underestimates the total number of COVID19 infections.
Recent studies bring into question the diagnosis of COVID19 myocarditis
A recent cardiac imaging study suggest myocarditis is not the major mechanism of cardiac injury after a COVID-19 infection.
An accompanying editorial notes “Data from COVID-Heart provide reassuring evidence that myocarditis, once predicted to be an emerging public health crisis attributable to COVID-19, is relatively uncommon even among hospitalized patients and is less virulent than predicted during the early days of the pandemic. It is likely that elevated cardiac troponin concentrations during COVID-19 in many patients do not reflect significant new myocardial injury and fibrosis, but rather cardiac troponin release from vulnerable hearts with pre-existing scar in the setting of severe illness”
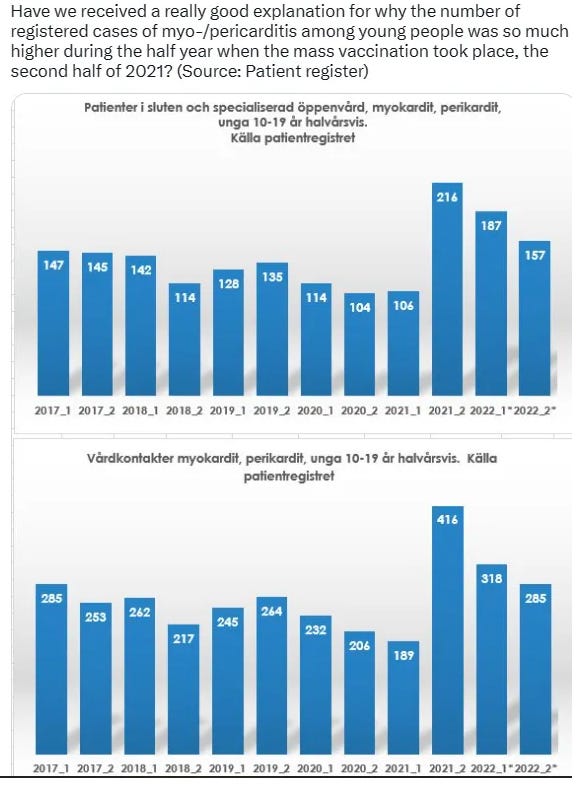
Data obtained by a record request from Sweden clearly demonstrate elevated rates of myocarditis in the time period after initiation of the COVID mass vaccination campaign, with no appreciable increase in the rate of myocarditis during widespread COVID in the year prior.
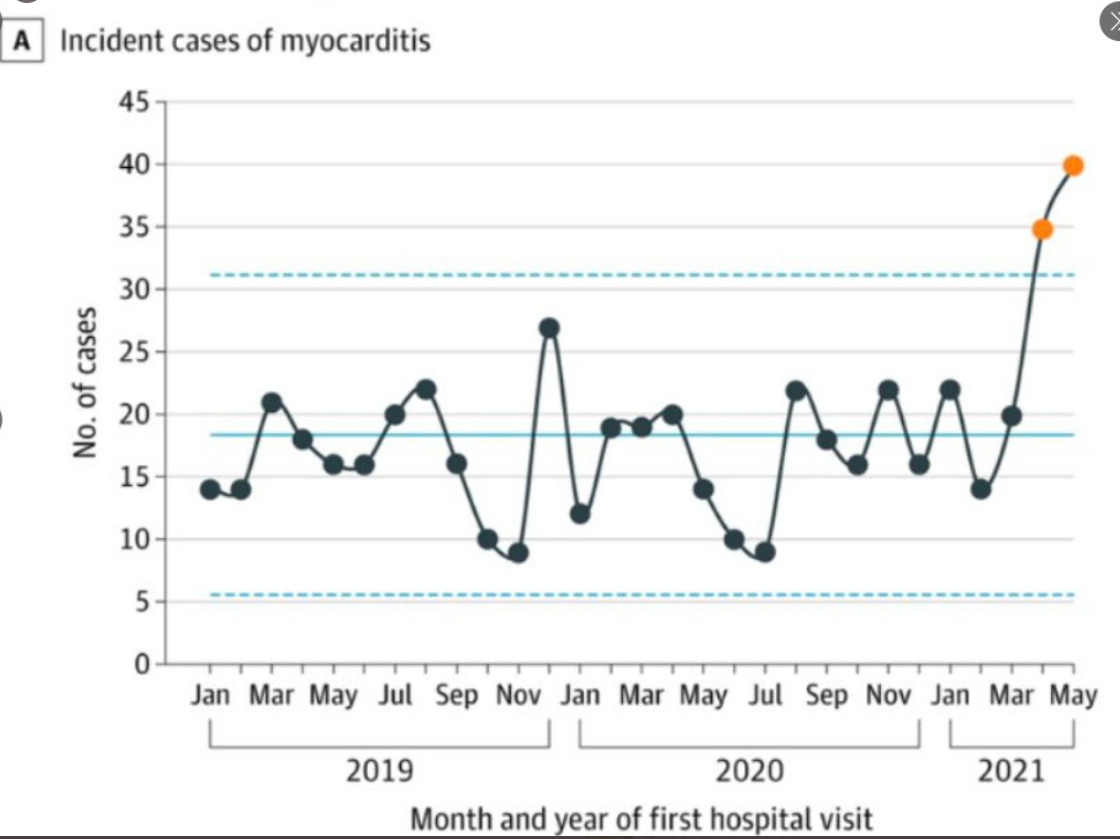
This spike in myocarditis diagnoses seen only after initiation of the vaccination campaign is corroborated by rigorous studies
6. requiring corroboration of a myocarditis diagnosis with the appropriate clinical context and cardiac imaging.
Recovery from a COVID infection confers strong, durable protection against future COVID infections
A systematic review and meta-analysis of prior infection with COVID suggests protection against re-infection “was very high and remained high even after 40 weeks.” The authors of this paper go on to suggest that “the immunity conferred by past infection should be weighed alongside protection from vaccination when assessing future disease burden from COVID-19”.
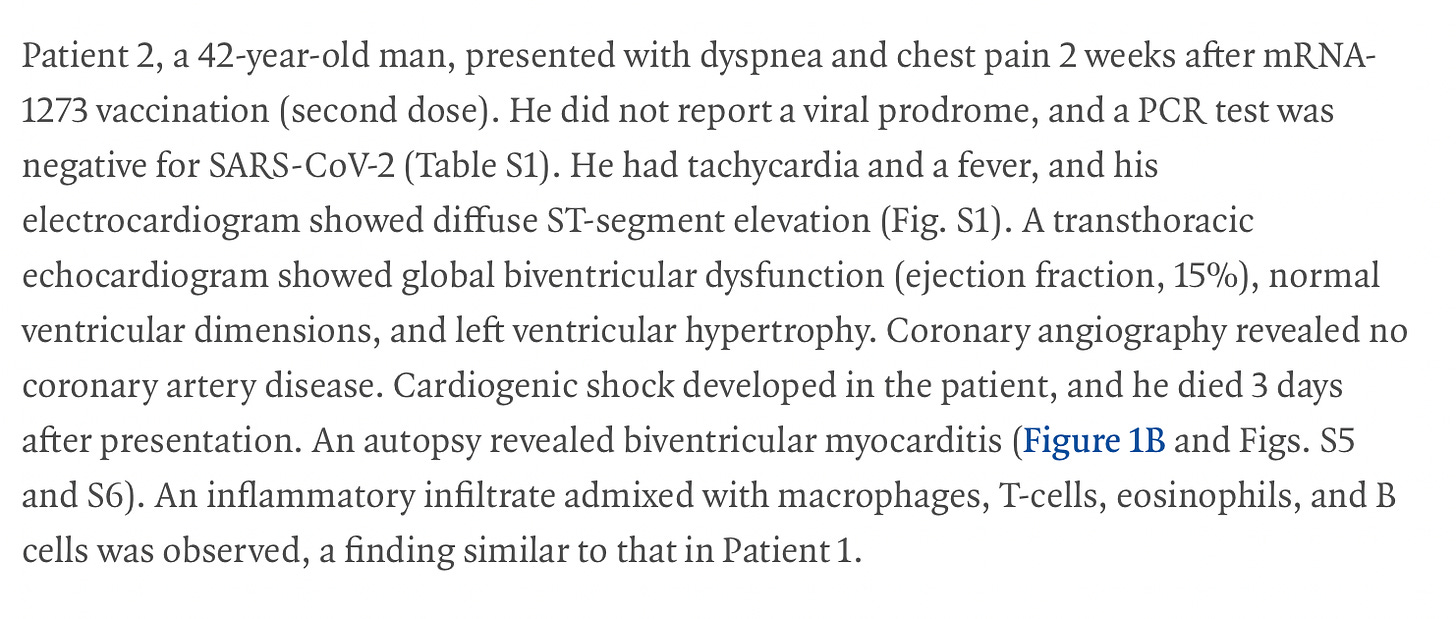
Vaccine myocarditis can be serious and life threatening.
The vast majority of cases of vaccine myocarditis requires hospitalization for monitoring for deterioration. While the majority of patients are discharged home to recover, the current recommendation is for recovering patients to avoid strenuous activity for 6 months. A majority of patients that follow up for cardiac MRI imaging are seen to have scar in long term follow up. There are also case reports of severe morbidity and mortality from vaccine myocarditis resulting in critical illness or death.
Prior episodes of vaccine myocarditis have been linked to an increased risk of myocarditis with future vaccinations
Two case reports from Australia describe myocarditis after administration of the Novavax vaccine to two young individuals who had recovered from mRNA vaccine myocarditis.
The two case reports from Australia aren’t even the first reports of Novovax myocarditis after mRNA vaccine myocarditis. In August, the CDC reported 29 cases of pericarditis, including five in persons with a history of pericarditis after mRNA COVID-19 vaccine;
Importantly, the Novovax vaccine is a protein-based vaccine that was hoped to not be associated with myocarditis as was noted with the mRNA vaccines. Unfortunately, these report of myocarditis occurring after Novovax delivery in patients who had a prior case of mRNA vaccine myocarditis suggests a history of vaccine myocarditis should serve as a contraindication to any future COVID-19 vaccines.
Summary / Recommendations:
Mr. Smith is a 31 year old man with no medical history. He emphatically denies any history of cardiopulmonary disease. He received his first dose of a Pfizer mRNA COVID-19 vaccine in June 2021. He subsequently describes having sharp chest pain over the next few weeks. He did not seek any medical evaluation at the time as he did not link the chest pain with the first dose of the vaccine he received. The pain resolved a few weeks later. He has had COVID twice, first in September of 2020, and his second time in January of 2023.
His cardiac testing completed to date consist of an electrocardiogram and an echocardiogram performed Feb 16th, 2023 that were both normal.
I think it is certainly possible Mr. Smith may have had myocarditis after the first dose of his mRNA vaccine. As I discussed with Mr. Smith, a cardiac MRI would not change my opinion on the matter as a normal result this many months from his original presentation would not rule out acute myocarditis. If he did have a case of vaccine myocarditis after his first dose of an mRNA vaccine, I think he would be at risk for developing myocarditis with another COVID-19 vaccination. I will note here that Mr. Smith did try to fulfill the mandate to complete a primary series of a COVID-19 vaccination by attempting to get a Johnson and Johnson vaccine. He was turned away by the pharmacists who noted the Johnson and Johnson vaccine was not approved to be given after a first dose of an mRNA vaccine.
As I have detailed, while most cases of vaccine myocarditis have not been shown to result in severe morbidity or mortality, there are clearly case reports of severe vaccine myocarditis. Especially given Mr. Smith has had two separate COVID infections, with his most recent infection in January of 2023, it is very unlikely that the unclear benefits of a second dose of a COVID-19 vaccine are outweighed by the risk of vaccine myocarditis.
I understand the committee has concerns beyond individual protection with regards to vaccination as it was hoped that vaccinations against COVID19 would reduce the likelihood of transmission of the virus and thus provide protection to the community in addition to the individual. As you know, the initial randomized control trials were not designed to test for reduction in transmission, and the degree of reduction in transmission is a matter of debate now. Beyond the unknown efficacy of the vaccines related to transmission risk, there does appear to be growing consensus about the equivalence of a prior infection from COVID and vaccination. The meta-analysis on prior infection referenced above prompted the Chairman of Medicine from UCSF, Dr. Bob Wachter to write :
Since nearly all unvaxxed have been infected by now (many>once), study lowers the case for vax mandates, since those w/ prior infection likely have protection not materially worse than if they were vaxxed.
It should also be relevant that Mr. Smith is a non-clinical, remote worker who has no direct contact with patients or other healthcare staff.
For all of the above reasons, I would respectfully ask members of the vaccine exemption committee to reconsider and grant Mr. Smith an exemption from the company’s vaccine mandate.
Yours Sincerely,
Anish Koka MD
Cardiologist
Philadelphia, Pennsylvania
Categories: Medical Practice