Somewhat ironically, I returned from Manhattan that same day to a waiting email from a colleague, forwarding me a rather excoriating critique of integrative medicine on The Health Care Blog, and asking me for my opinion.
The juxtaposition, it turns out, was something other than happenstance. The Cleveland Clinic has recently introduced the use of herbal medicines as an option for its patients, generating considerable media attention.
Some of it, as in the case of the Katie Couric Show, is of the kinder, gentler variety. Some, like The Health Care Blog — is rather less so. Which is the right response?
One might argue, from the perspective of evidence based medicine, that harsh treatment is warranted for everything operating under the banner of “alternative” medicine, or any of the nomenclature alternative to “alternative” — such as complementary, holistic, traditional, or integrative.
One might argue, conversely, for a warm embrace from the perspective of patient-centered care, in which patient preference is a primary driver.
I tend to argue both ways, and land in the middle. I’ll elaborate.
First, I am a card-carrying member (well, I would be if they issued cards) of the evidence-based medicine club. I am a conventionally trained Internist, and run a federally funded clinical research laboratory. I have taught biostatistics, evidence-based medicine, and clinical epidemiology to Yale medical students over a span of nearly a decade. I have authored a textbook on evidence-based medicine.
But on the other hand, I practice Integrative Medicine, and have done so for nearly 15 years. And I represent Yale on the steering committee of the Consortium of Academic Health Centers for Integrative Medicine.
Odd as it may seem, I consider these platforms entirely compatible. I did not go into Integrative Medicine because I believe “natural” is reliably better or safer than “scientific.” I respect the often considerable prowess of modern medical technology and pharmaceuticals.
And, frankly, I have never much cared whether a therapy derived from a tree leaf, or a test tube. I have cared about whether it was safe, and whether it was effective.
As an Internist taking care of patients for many years, one thing was painfully clear: I could not make everyone better. And while this deficiency might have been my personal shortcoming, it was much more than that. Modern medicine couldn’t make everyone better.
We tended to fall down particularly when it came to treating chronic pain, or chronic fatigue. We tended to stumble rather badly over any condition with “syndrome” in the title (as opposed to a “disease,” a “syndrome” is a description of symptoms generally lacking a clear explanation).
Integrative Medicine — a fusion of conventional and “alternative” treatments — provided patients access to a wider array of options. So, for instance, if medication was ineffective for anxiety or produced intolerable side effects, options such as meditation, biofeedback, or yoga might be explored.
If analgesics or anti-inflammatories failed to alleviate joint pain or produced side effects, such options as acupuncture or massage could be explored.
The array of potential options extends, of course, to herbal remedies and nutriceuticals as well — the apparent focus at the Cleveland Clinic. And, more controversially, it potentially extends to modalities that conventionally trained clinicians find implausible, such as homeopathy or energy therapies. I won’t get too deep into such weeds today, but have done so before.
Here are a few key considerations from my perspective.
1. Evidence is not a reliable differentiator of conventional and alternative medicine. By the standards that now prevail, more than 50 percent of conventional medical practice is not truly “evidence based.” Some years ago, colleagues and I were charged in a CDC grant to chart the evidence related to complementary and alternative medicine.
We would up inventing a technique called “evidence mapping,” since adopted by the World Health Organization and applied to an international traumatic brain injury program. Our finding was that in the realm of alternative medicine, some practices are rather well studied, some are understudied and some unstudied. Much like conventional medicine, in other words.
2. To the extent that evidence does differentiate conventional and alternative medicine, it’s often because — in the pursuit of evidence — cart and horse routinely swap positions and money cracks the whip. If the horse pulled the cart, then what gets studied would be what is needed, and what looks promising. But in our world, what gets studied often begins with what can be patented. It now costs nearly a $billion to bring a new FDA approved drug to market.
The only rationale for spending that much is the likelihood making back much more — and that only occurs when the product in question is exclusive and propriety, i.e., patented. There is a classic demonstration of the power of this influence.
More than a decade ago, a study of about 50 people followed for about three months was used to “prove” that coenzyme Q 10 was ineffective for treating congestive heart failure. At about the same time, a study of nearly two thousand people followed for years proved that the proprietary drug, carvedilol, was effective. The difference at the time was not really evidence — it was money.
A great deal more money was spent on the carvedilol trial — because no one can patent coenzyme Q 10.
More than a decade later, we now have evidence that coenzyme Q 10, when added to standard therapy for heart failure, can reduce mortality by as much as 50 percent. That is a stunning effect for something that has been “alternative” medicine all this time, and was declared useless by the conventional medical establishment.
Unless we are willing to practice money-based medicine, or patent-based medicine, we are obligated to recognize that the playing field for generating evidence is not level. It is tilted steeply in favor of patent holders.
3. Evidence is not black or white. It comes in shades of gray. Clinical decisions are easy if a treatment is known to be dangerous and ineffective, or known to be safe and uniquely effective. But what if a given patient has tried all the remedies best supported by randomized clinical trials, but has “stubbornly” refused to behave as the textbooks advise and failed to get better?
Or what if a patient just can’t tolerate the treatments with the most underlying evidence? One option is to tell such a patient: See ya! But I think that is an abdication of the oaths we physicians took. When the going gets tough, we are most obligated to take our patients by the hand, not wave goodbye.
To address this very scenario, colleagues and I have developed and published a construct that examines therapeutic options across five domains: safety; efficacy; quality of evidence; therapeutic alternatives; and patient preference. If a patient is otherwise running out of options and is in need, trying something that is likely to be safe and possibly effective — makes sense.
If there is something that is likely to be safer and more effective, then that should be used first.
But by recognizing and prioritizing the obligation to blend responsible use of evidence with responsiveness to the needs of patients that often go on when the results of large randomized, clinical trials have run out — we can wind up, inadvertently even, in the realm of Integrative Medicine.
That’s how I got here.
The needs of my patients led and I followed. And yes, the wider array of treatment options I can offer working side by side with my naturopathic colleagues absolutely does mean I have been able to help patients I otherwise could not.
Integrative Medicine should not involve a choice between responsible use of evidence and responsiveness to the needs of all patients. It should combine the two. We should do the best we can with the evidence we have, but recognize that high quality evidence may start to dwindle before our patient’s symptoms start to resolve.
We should resolve to confront this challenge with our patients, not leave them to fend for themselves.
The belief that treatments are intrinsically better just because they are “natural” is fatuous and misguided. Smallpox, botulinum toxin and rattlesnake venom are natural. Nature is not benevolent.
But the belief that conventional medicine is reliably evidence-based is equally fatuous. Much of what we do is simply tradition. And much of the evidence we get is more about money than other imperatives. Often in the world of alternative medicine, the problem is not evidence of absent effects — but a relative absence of evidence, in turn engendered by an absence of patents and financial incentives.
The history of coenzyme Q10 is a precautionary tale if ever there was one.
Integrative Medicine is not an invitation to supplant evidence with wishful thinking. It is an invitation to a wider array of treatment options, and the prospect of effectively addressing patient need more of the time. Realizing such potential benefits — at the Cleveland Clinic, or anywhere else — requires both open mindedness and careful skepticism.
It calls for a holistic view of the full array of therapeutic options, and the recognition that both conventional and alternative medicine are home to baby and bathwater. Differentiating can be hard — and we and our patients should be confronting that challenge together.
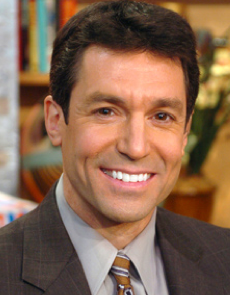
David Katz, MD, MPH, FACPM, FACP, is the founding (1998) director of Yale University’s Prevention Research Center, and author of recently published book, Disease-Proof. This piece first appeared at The Huffington Post.
Categories: Uncategorized










This is the best summary I’ve seen of what is actually happening in EBM and how it affects the practice of allopathic and other systems of medicine. Thank you.
Anoop Kumar, MD
Yes, another informal logical fallacy
the idea of “traditional treatments that… have been used for centuries.”
__
a.k.a “Argument from Tradition”
Grrrr…. THCB is blocking my links again.
See my Dec 4th REC Blog post on Mario Bunge.
Dr. Katz, I once again genuinely thank you for your continued discussion in the matter. I can absolutely assure you that I care not from where or whom a therapy comes – so long as I can be convinced it can help my patient I will use it.
I find it interesting that you disagree on the topic of medical students learning the hierarchy of evidence. In my first year of medical school we had an entire year-long course on it, with exercises, projects, and questions on our exams pertaining to it. Similar for a number of friends and classmates at other medical schools. Perhaps things have changed since you graduated? Or perhaps my small sample size is biased. In any event, I wholeheartedly agree that it should be taught to all medical students in a rigorous manner and with an added emphasis on Bayesian frameworks which incorporate all relevant evidence, including bench sciences, to inform decision making. The idea that only RCTs and meta-analyses can inform decisions seems perverse to me (and indeed has been dubbed “methodolatry” by some) and is not at all what any of my colleagues and classmates think is appropriate.
But that hierarchy of evidence cuts both ways. For example, when there are equivocal clinical studies in homeopathy, we can look at the bench sciences to inform us that the prior plausibility is so low that equivocal studies can be rightfully regarded as resoundingly negative. A point on which you have failed to expound – your own admitted use of homeopathy with patients.
You certainly make a valid point about perverse incentives (as I like to call them) nudging us against non-proprietary, low profit modalities. There is a very good reason why my institution has banned drug company lunches for many years and why I support such initiatives. But that still does not justify the use of unproven or disproven modalities in patient care. We can – and should – lament when we are at a lack of tools and knowledge to help our patients, but I fail to see how picking something at random is any better than admitting the limitations of our current abilities. It seems to me much more productive and better for our patients to instead focus our efforts on improving the process.
Which brings me to the idea of “traditional treatments that… have been used for centuries.” I wholeheartedly disagree that this is a valid surrogate to use for establishing the probability of safety. To use a cliche, bloodletting was used for many thousands of years and it is clearly not safe nor therapeutic. But in a more serious example (of which there are myriad) I would like to draw your attention to aristolochia. That is an herb that was used for at least many hundreds of years, if not thousands, and is in the Bencao Gangmu, now known as the Compendium of Materia Medica of Traditional Chinese Medicine (TCM). The Bencao Gangmu was compiled in the 16th century and there is evidence of the use of aristolochia dating back to the 1st century CE and even ancient Egypt. By your argument one would expect that to be an excellent establishment of a high probability of safety. Yet, in 1993 it began to be noted that people who ingested this herb had unusually high levels of urothelial cancers. A decade later it was noted that so-called “Chinese Herbs Nephropathy” and “Balkan Endemic Nephropathy” are likely the same thing and finally in 2013 it was demonstrated that aristolochia is a potent carcinogen, with it’s effects not limited to patients ingesting it, but also the herbalists producing it. As is noted in this study a full one-third of the population of Taiwan was prescribed something with aristolochia in it. In the words of the authors:
By your proposed approach to judging the potential safety of therapeutics, aristolochia would be a reasonable therapeutic to try (prior to 1993 and arguably up until the early 2000’s) as it meets all of your requirements as outlined in your CURE paradigm: it has been used by many cultures for thousands of years (probable safety), it would come on the recommendation of a person trained in an accredited program, with national certification, standardized education, and government regulation and licensure (an acupuncturist/oriental medicine specialist; possible efficacy), and unclear scientific evidence of efficacy (ambivalent evidence of efficacy prior to 1993). In our hypothetical patient for whom we are low on options, it could not have been argued by you that trying aristolochia would be anything but acceptable.
And yet, we would have been exposing our patients to a greatly increased risk of cancer with no evidence of benefit and no rational reason to assume there would be, beyond TCM use based on pre-scientific approaches to pathophysiology.
My own background includes an undergraduate degree in medical anthropology in which I studied many different systems of medicine, as well as advanced coursework in molecular pharmacology, and post-graduate research in pharmacognosy (specifically investigating the anti-senescent properties of botanical extracts). This is but one of many examples of the pitfalls of assuming safety based on proxies such as traditional use and an illustration that relying on traditional use as indications for therapy is almost the same as walking into a field and picking a random plant to give your patient. Even thousands of years of use is worthless if the results aren’t carefully recorded. That’s why we invented science in the first place.
The key to your argument is “when risk is nil” – but that is not something I believe can be established based on the methods you are proposing. And it is well demonstrated that something is more likely to harm or do nothing than be of any benefit. Else we would have our patients chewing on yew trees and periwinkle flowers and the field of pharmacognosy would be of very low value.
I would posit that in cases of few options the best thing we can do to genuinely help our patients is to support and empower them, not give them placebos or experiment on them. If I had tried aristolochia and later learned that I was likely the cause of my patient’s urothelial cancer and nephropathy that would seem to outweigh any slim chance of benefit for both of us.
In conclusion, I do fully agree with your conclusion in principle. But I disagree that a “more fluid form of evidence” as you describe is the way to achieve those laudable goals. There is no such thing as a free lunch and with any intervention that could possibly have benefit there is also necessarily the possibility of harm. Without due diligence beforehand, we have absolutely no idea where that balance may lie and are betting on the benevolence of Mother Nature and the wisdom of pre-scientific thinkers. Those are not bets I would take, if I were on the other side of the exam table.
I disagree that every medical student learns to work along a hierarchy of evidence, turning to the ‘next best thing’ most likely to help a patient in need. I think many learn that there is either a meta-analysis or large RCT to back up a therapy, or it should be ignored entirely.
I would also note that forces in our culture conspire against the utilization of non-proprietary, low-profit modalities. It’s just naive not to notice this, or think otherwise.
Finally, there are ‘traditional’ treatments that in many cases have been used for centuries. While the accumulation of such experience is no substitute for randomized trials in proving efficacy, it can serve quite well to establish the high probability of safety. That, of course, is an important consideration- since what matters ultimately is the risk/benefit ratio. When risk is nil, and options are few- even a slim chance of therapeutic benefit may be worth taking.
What I am pleased to see is that we are not really debating evidence, or nomenclature- we are debating methods of practice, HOW to apply evidence to greatest effect. That, I believe, is the correct focus. The notion of ‘this or that,’ ‘conventional or alternative’ is a distraction. What we should care about is: what is the best thing I can offer any given patient in need, and how do I get there from here? Were we all to devote our efforts to that challenge, I think we- and more importantly, our patients- would benefit considerably.
Once again, thank you for your time Dr. Katz.
Superficially we certainly agree. I wholeheartedly agree that ultimately getting the job done is what matters and there are, as you know, many barriers to achieving that in practice beyond the limitations of scientific knowledge.
Your CURE construct is also superficially agreeable. But it also strikes me as excessively vague. It also, once again, does not jibe with your use of homeopathy. All of your categories include a patient preference for something that works. Homeopathy cannot work.
It seems that here we disagree on the what constitutes that scale of evidence. Homeopathy is a good litmus test because it cannot possibly meet any definition by your own rubric that exceeds a “never” in terms of utilization frequency. Yet you seem to have used homeopathy at the suggestion of a naturopath, which goes against your own (albeit vague) recommendations.
Which raises another point from the paper you linked – your standard is:
…essentially nonexistent. And certainly not at all based on actual scientific legitimacy. By this standard if a sect of voodoo priests had enough lobby power in Congress they would be deemed worthy to collaborate in patient care and offer suggestions for treatments. And scientific legitimacy is demonstrably not a requirement for accreditation, standardized education, or government regulation. Bob Jones University is a prime example of this, as is Bastyr and the entire field of naturopathy, which you none the less seem to embrace. You even say:
Once again we agree in principle, yet in execution something is profoundly lost. The entirety of your argument – and this particular paper – boils down to nothing more compelling or novel than saying we should follow evidence, starting at the top and working our way down as needed. This is something I knew before starting medical school but every first year student learns (or should at least). The only difference is that you seem to have no limit as to how low down the evidence totem pole you are willing to go. If a naturopath recommending homeopathy seems like a reasonable option, why not every old wive’s tale that any random person can conjure up?Do we not owe it to our patients to do more than just flail at them with every nostrum we can throw at them, no matter how ridiculous?
There are limits to medical and scientific knowledge. Limits that are continually pushed farther and farther out. Not fast enough, but we can (and should) always feel that way. When we’ve reached those limits, abdicating our responsibility to our patients to understand, to empower them to cope and manage their condition in favor of what are nothing more than wild guesses at best is no better than the heavy paternalism of our forebears.
If you genuinely do wish to “get the job done” (and I truly believe you do, as do I and all of our colleagues) abandoning the principles of rigorous scientific inquiry to the ilk of naturopaths, acupuncturists, TCM practitioners, and chiropractors is not the way to do it. One does not move forward by traveling back in time to pre-scientific nostrums, nor do we improve patient care by abandoning standards.
I still genuinely fail to understand what value your proposed integrative medicine adds to patient care beyond treating ourselves and the patient to placebo medicine.
Actually, I prefer no separate category. What matters is how we proceed when we have exhausted all of the ‘high quality’ evidence, but our patient’s need remains inadequately addressed. Call that CAM, or ‘the next best thing,’ or the ‘art’ of medicine. The rubric matters little; getting the job done matters a lot. The method we use in my clinic is the CURE construct on p. 27 of this paper-
http://www.iom.edu/~/media/Files/Activity%20Files/Quality/IntegrativeMed/Preventive%20Medicine%20Integrative%20Medicine%20and%20the%20Health%20of%20the%20Public.pdf
Dr. Katz, thank you for taking the time to respond.
I am generally overly wordy so I’ll try and be concise as best I can.
In essence, I am reading your argument as saying that in the face of immediate patient need we should lower the standards of evidence to allow for less evidence based therapies to be administered to our patients and that further this is what “CAM” allows us to do. In other words, “CAM” is nothing more than a term for creating a double standard in which therapies with inadequate evidence to support them can be ethically administered to patients outside of a clinical trial.
I take multiple issues with this approach and this argument.
First and foremost it does not at all explain how you can possibly find homeopathic treatments to fit into this proposed paradigm. By what possible rationale can you assert that homeopathy is a “promising, but not truly ripe” modality? If there is one “alternative medicine” that can be less promising I cannot think of one. This can be repeated for nearly all things labeled “CAM”, including many of which you are on public record as advocating (or at least having administered to patients).
But to address the actual argument you are offering here, it still fails to provide any reasonable rationale for the notion of calling these lower-evidenced therapies “CAM.” Why create a separate category? If the premise is simply that the (admittedly flawed) machinations of medical research are too slow in certain regards, then it makes no difference whether something is “CAM” or not. There is no special validity that somehow grants a higher prior plausibility to something labeled “CAM” than any other random thing you may wish to experiment on patients with (and make no mistake, providing an a treatment in the absence of evidence is experimentation). In fact, you explicitly make that argument but to a degree I am forced to disagree with. Was it not you who said:
Neglecting the fact that you are attempting to say that everything is so equally implausible as to be equally plausible, does this not directly contradict the idea of giving an special quarter to something labeled “CAM” as being somehow more likely to be useful in the absence of evidence?
So how on earth does one pick from the literally limitless possible therapies without evidence to experiment on our patients with? And how would you know if it worked? You say:
Besides the fact that there are anecdotes for everything from alien abductions to mind control, you simply cannot say “it worked” because such interactions can, by definition, only demonstrate correlation, not causality. To say otherwise is to abandon the science you claim you believe in.
One place we do agree is when you say, “patient need is immediate, and data generation is slow, there is a need to make the best use today of the data we have today.” But if you are resorting to using homeopathy and listening to naturopaths then you are very clearly not making the best use of the data we have today. At that point one may as well be trying to use unicorn tears to address immediate patient needs.
The failures and flaws of the current research paradigm – the one that declared CoQ10 dead – do not magically validate incredibly implausible and unproven claims. As Ben Goldacre said, flaws in aircraft design does not mean that magic carpets can fly. I would argue that using CAM as a crutch to defend what would otherwise be unethical patient care – either providing placebo medicine or doing experimentation on humans without IRB approval – is contra to your stated claims of giving patients needed treatments in an accelerated timeframe.
We disagree on a number of points, clearly- but I will only address one. The difference between, for instance, co Q10 as “alternative” medicine and co Q10 as “conventional” medicine is measured in years, if not decades. Yes, the research in this case did eventually get done- but it was ten years after under-powered studies were used to declare the ‘co Q10 for heart failure hypothesis’ dead. Does that happen with a conventional drug: it is studied in too small a sample, little is seen, and the ‘hypothesis’ that the drug could work is declared ‘dead’? It does not.
You seem to be dismissing the significance of the timeline. For any given patient in need of an option today, data that will ripen ten years from now are of no real use. What “alternative” medicine does is apply promising, but not truly ripe, data so that today’s problem can be addressed today. The down side to this, of course, is that the agent in question may be ineffective, and potentially dangerous. The up side is that when they are right, they are right ten years or more before we are.
The less profitable the product, the longer the timeline to get a critical mass of research done.
Because patient need is immediate, and data generation is slow, there is a need to make the best use today of the data we have today. That simple imperative leads to therapies for which the evidence is suggestive, but not truly ready for prime time- and thus, integrative medicine. The need to work diligently to differentiate baby from bathwater is, I think, self evident. Best- DK
Well said, BobbyGVegas.
Oops, the browser template chokes on inequality symbols. Let me re-state:
p(s) LT 1.0
p(a) LT 1.0
ergo,
p(s) x p(a) GT p(s)
“Which brings me to “integrative medicine.” What, exactly, is being integrated?”
___
I guess when you “integrate” the unscientific with the scientific, you somehow — in contradiction to the “conjunctive fallacy” — STRENGTHEN science.
p(s) < 1.0
p(a) p(s)
‘eh?
Except that your clear outcome can only demonstrate a correlation, not a causation. And any student of the sciences should be able to inform you of how easily we can be led astray by that. Which is why an n=1 trial is worth extraordinarily little except, in rare cases, to prompt further inquiry.
Appeals to authority notwithstanding, alternative medicine does not fit that idea to a T. It is also not universally true – so much so that it is even an informal logical fallacy known as the argument to moderation. If I were to argue that 2+2=4 and you that 2+2=5, does it stand to reason that the correct answer must be that 2+2=4.5? Of course not.
In order to argue that there is something valid in an argument that the truth of a matter is somewhere in between two opposing viewpoints there must also be an (relatively) equal amount of evidence to support both sides. Since Dr. Katz has publicly admitted his wont to resort to homeopathy as part of his “integrative” approach it seems a reasonable point to make: the entirety of science clearly, unequivocally, and vociferously tells us that homeopathy cannot possibly work. The clinical data is consistent with this as well. So does that mean that the truth of its efficacy is somewhere in between and that it works sometimes, or in some people, or to some lesser degree (as Dr. Katz would have us believe)? No. There is a clear cut answer, and it truly is “nothing.”
John, you say:
I am saying that there makes no sense to have such a category in the first place. Particularly not as a means to enable the proffering of therapies with a lack of evidence. What purpose does it serve to call something “alternative medicine?” What does that even mean? Alternative to what? Medicine is supposed to be rooted firmly in science and evidence. From that vein we can draw on anything to give us knowledge and tools. I don’t care – and neither does anyone else like minded – whether that knowledge and tools comes from ancient Chinese practices or a plant in the Amazon or from the latest breakthrough at CERN. On that, Dr. Katz and I agree.
So yes, ask questions. But do not presume the answers or use unproven or disproven modalities on patients because you simply can’t think of anything better to do.
Which brings me to “integrative medicine.” What, exactly, is being integrated? If a therapy has a sufficient evidence base it should be used in concordance with that evidence. It is simply “medicine” at that point. Is “integrative medicine” integrated medicine with medicine? No, it is rather explicitly integrated so-called “alternative medicine” with actual medicine. What makes something “alternative”? Only one of two things – it either has evidence that it doesn’t work or simply has not been adequately studied. In either case it should not be “integrated” into medical practice.
Diet, exercise, yoga, vitamins, meditation, etc are not alternative. They have an evidence base with a rational as to why and how they work and the limitations therein. Trying to assert that advising our patients to exercise is “integrative” is a disservice to the very rigorous and diligently studied field of sports and exercise physiology. To then use it as a foothold to try and bring in profoundly inane modalities like homeopathy since they are both “alternative” is nothing more than disingenuous and intellectually dishonest.
As mentioned before I am an anecdotal case in which there was a clear outcome — 4 years of daily meds, following by the “alternative” intervention” followed by complete discontinuation. I realize N of 1 does not a study make, but I think Dr. Katz’s middle ground is the right answer.
As for your answer, it seems too dogmatic under the circumstances. When I taught economics (at Harvard, as long as commenters seem to be sharing their Harvard credentials), I used to tell the students: “In economics the answer is almost never ‘all’ or ‘nothing.’ ” Alternative medicine would seem to fit that observation to a T.
The reality is that there isn’t enough time, money, and humanity available to test every conventional or alternative therapy and rate its effectiveness and thus make thoughtful decisions about access to it, with or without reimbursement. Forget about rating its value, which will vary between patients.
It seems to make that we are also losing sight of two other important issues: the placebo effect and the value of experience. For my late father, acupuncture proved to be an important source of relief from intractable back pain, when no other therapy proved useful (late 1960s, early 1970s). Was it placebo or did it actually have an effect? I don’t know; all I know is that it worked.
The only thing we are reaching the limits of in modern medicine is sanity and good judgment.
Lucky that we now have the technology to quantify a lot of these questions cheaply and reasonably quickly by gathering data in ways that was impossible just a few years ago.
Andrey and friends: doesn’t it make sense to impose a cease fire in this war – at least temporarily so this can be studied. Or is it your position that the case is officially closed on ALL forms of integrative and alternative medicine? I’m willing to accept that many of these practices are myths and various forms of magical thinking as you put it, but that’s inevitable. For every answer we ask a hundred and fifty questions, or some equally improbable ratio.
How is science supposed to work if we don’t continue to ask questions? How is it supposed to work when we don’t know what we know and what we don’t know?
Point #1 is nothing more than a tu quoque argument. Regardless of whether your statistics are actually correct (and they are arguably not) it has nothing to do with the question at hand. Whether “conventional medicine” is 100% evidence based or 0% evidence based does not endorse nor impugn so-called alternative medicine.
Point #2 is valid but incomplete. Yes, undoubtedly patentability and profit drive pharmaceutical development. And this does include some perverse incentives. However, it is incorrect to say that natural products are unpatentable. Even CoQ10 products can be patented – either by brand name or by process of development. Tylenol is an excellent example – it is generic, yet the brand still exists and now IV acetaminophen is available and at extremely high cost. The key is that there was some actual evidence to support its use in control of post-surgical pain. All from a widely known generic drug that in and of itself is not patentable. So this argument falls flat.
But the truly key piece that is missing in your understanding and analysis is by far the most important – what is the likelihood that it will work. Things that have billions of dollars invested in their development are not going to be utterly implausible like homeopathy or some random herbal decoction pulled from the thoughts of a pre-scientific thinker in ancient China. So yes, the profit motive does end up steering research away from some viable sources, but by in large it steers away from all the ones least likely to work. Yet also happen to be the ones you seem to favor.
Additionally, your own example of CoQ10 undermines your argument. Something that is difficult to monetize is more likely to get short shrift, no doubt. But when it has some rationale and a little bit of evidence that it actually works it gets researched. Otherwise you wouldn’t have the example to tell us. You’ve given not an example to support your argument, but one to show that even with the known flaws of the system it still does work (though it can always work better and we should strive to improve at all times).
And point #3 is a straw man. One intended to obfuscate the point and try to argue that because clinical medicine is hard and sometimes confusing, anything goes. There is more to evidence than just RCTs, so when our available treatments fail our patients the answer is not to resort to magical thinking and throwing stuff at the wall until it sticks, but to actually use the other available evidence at our disposal. Doing so would make the idea of offering a patient homeopathic nostrums not just silly but downright unethical. Sticking your fingers in your ears and claiming that you just don’t know how it works but it does is not a professional nor rational way to approach patient care. There are reasons why homeopathy cannot be anything more than a placebo so well verified that to think otherwise shows a profoundly disturbing level of ignorance, whether willful or not.
Ultimately your entire argument boils down to the idea that when the limits of modern medicine have been reached, magical thinking and randomly picking therapies out of a giant grab bag are not just reasonable but the only alternatives, dressed up in the guise of patient centered care. Both of these ideas are patently false. And patient centered care is independent of the question of the evidence base for therapeutic approaches.
We can do much better for our patients than treating them like children and pretending magical nostrums and incantations do something for them. Doing as you suggest is nothing more than the overbearing paternalism of our forebears and has no place in truly patient centered care.
The two most important phrases in this very useful post are: “money cracks the whip” and “Much of what we do is simply tradition.” Interestingly, in terms of reimbursement, tradition drove payment and still does.
The thing that troubles me most about the conventional vs. alternative approach is our inability to talk about the elephant in the room: reimbursement. Because we reimburse by tradition (and not evidence) for many things that physicians do, should we give the same deference to alternative therapies and their practitioners? Clearly, they would love that opportunity because once they’ve gained entry to the big tent of tax-subsidized reimbursement, it will be nearly impossible to remove them.
And, if we want to submit to alternative therapies and their providers to a higher bar for reimbursement than we ever did conventional providers, what does that say about our devotion to both equity and evidence? Can we chew health policy gum and walk at the same time? Can we both find ways to squelch unproductive conventional clinical practices (and stifle the squealing of all the poor, impoverished specialists) and at the same time do really meaningful clinical trials of alternative therapies so that we embrace what works instead of just “well, this is the way we’ve always done it.” I am dubious, and over the past 50 years, as a culture, we’ve been given no reason to think that the medical-industrial complex can sort this out equitably and with integrity.
There is no such thing as alternative medicine or traditional medicine. There is only medicine with evidence and medicine without evidence. You are quite right that evidence does not differentiate the two, there is unclear thinking in both, inference stretching the conclusion of the empirical proof. The question is where are you comfortable setting the bar.
As far as applying the data rationally in the context of the patient’s preference, that is an old idea. It was first described by Donabedian under the concept of optimality.
Like you I am very firmly in the undecided camp. There are pluses and minuses. I myself have benefited from alternative medicine in that i had been taking Prevacid every day for 3 years to control indigestion. Then I was in a local supermarket and asked one of the employees where something was located. He said he didn’t know because he didn’t work in the store but was rather restocking the shelves with his company’s product.
I thanked him and began to walk away. Out of the blue, totally unprompted, he asked: “Do you ever get indigestion?” Well, needless to say I answered that I did. Turned out he worked for Dannon and gave me a coupon for a free eight-pack of their recently introduced product Activia.
That was 4 years ago and I haven’t taking a Prevacid since. (However, I have also used acupunrcture and chiropractic at various times for various reasons, to no effect.)
My issue with the Cleveland Clinic was about disclosure and how these products are positioned, not the herbal offerings themselves. If they were a bit more measured and objective in how they positioned these offerings, I would be completely on board with them, not that my opinion matters.
The philosophy of integrated medicine in medical science is totally a complete health care of the patient. Definitely, this evidence based medication strategy is good because we can not guarantee any treatment 100% successful. Yes, we can do the best for our patient if we follow this complete strategy. Only focusing on disease is not a perfect way. We should focus overall health of the patient. We should see every possible aspect of the available ways of treating the condition.