By ANISH KOKA and VIRAL MYALGIA
A number of colleges have mandated boosters for students returning to campus this fall. There are some points parents, teenagers, and whoever is coming up with policies at colleges may want to consider. Since no one has thought fit to actually generate any clinical data on boosters in college kids because of the continuous state of COVID emergency we have been in since early 2020, we are left to try to extrapolate from a vast amount of ecological data and surrogate endpoints.
While it would be impossible to include every single study ever done on the matter, there is clearly enough data to argue against their being the overwhelming scientific consensus that would be needed to underpin a policy that essentially forces individuals to receive a medical therapeutic.
- Strong evidence prior infection / prior vaccination is protective.The mandates do not take prior vaccination or recovery from a prior infection into account. This is a mistake. At this point, 97% of Americans have some protective immunity from either vaccination or infection. Recent data in a post-Omicron infection sample, shows that those with prior infection, with or without associated vaccination, have a robust rise in neutralizing antibodies after an Omicron infection. Indeed, those who were vaccinated alone with no prior infection had modal titers similar to those who were unvaccinated. In this same study, 47% of the vaccinees had an mRNA vaccination within the preceding 3 months and 40% had been boosted. Furthermore, those with a prior COVID infection had evidence of a much more robust immune response in the respiratory tract compared to vaccinated individuals.
- Boosters do not durably stop transmission or infectionUnfortunately, while there is some data that booster vaccinations cut the risk of contracting Sars-cov2 variants by roughly half, this protection appears to rapidly devolve over time as demonstrated by the significant variant waves that heavily boosted countries have demonstrated. A large CDC study with data from New York and California also found no extra benefit against severe disease from vaccination following infection.A large Qatari study noted BNT162b2 effectiveness was highest at 46.6% (95% CI: 33.4–57.2%) against symptomatic BA.1 and at 51.7% (95% CI: 43.2–58.9%) against symptomatic BA.2 infections in the first three months after the second dose, but declined to ~10% or below thereafter. Effectiveness rebounded to 59.9% (95% CI: 51.2–67.0%) and 43.7% (95% CI: 36.5–50.0%), respectively, in the first month after the booster dose, before declining again.
- Immunity following infection is durableA healthy immune system mounts an effective response to SARS-CoV-2 infection and this response persists over time. A recent July 2022 publication where 96.7% of study participants had mild or asymptomatic infection shows that children and young adults mount a robust antibody response that will fade with time, but remains measurably present. Once again this speaks to an expected pattern of less severe disease with any subsequent infection. This study reinforced prior research that measured these responses up to 12 months. The stimulation of an immune response after a mild infection can even be demonstrated in the absence of actual seroconversion (detectable prior infection by antibodies) at the level of T-cells. The presence of effective immune memory, both humoral (antibody) and cellular components, after even a mild SARS-CoV-2 infection is no longer a matter of debate. One might be tempted to argue that repeated boosting can permanently suppress infection. Unfortunately, all available evidence suggests that this increased protection from infection is transient. A recent publication from Iceland has offered unique insights into what we can expect with post-Omicron reinfections in different vaccination categories. While there were significant problems with possible ascertainment bias and grouping of unvaccinated with 1 dose recipients, the authors found.Surprisingly, 2 or more doses of vaccine were associated with a slightly higher probability of reinfection compared with 1 dose or less. This finding should be interpreted with caution because of limitations of our study, which include the inability to adjust for the complex relationships among prior infection, vaccine eligibility, and underlying conditions.A more robust nationwide study from Qatar, once again, provides corroborating evidence for the potency of prior infection. Per the authors:No discernable differences in protection against symptomatic BA.1 and BA.2 infection were seen with previous infection, vaccination, and hybrid immunity. Vaccination enhanced protection among persons who had had a previous infection. Hybrid immunity resulting from previous infection and recent booster vaccination conferred the strongest protection. [All provided excellent protection against severe outcomes.
- Boosting repeatedly against the original strain may have immunologic downsidesPer an NIH study, Omicron specific boosters did not elicit increases in Omicron specific neutralizing antibodies which is a concerning finding for a process called “imprinting”. This non-fringe opinion cited by vaccine expert Dr. Paul Offit in a New England Journal of Medicine editorial describes a process where the immune system gets locked into its first response to an infection, and is less able to respond to subsequent infections.
- Young college age men are a high-risk demographic for vaccine associated myocarditismRNA vaccine associated myocarditis/myopericarditis is an uncommon, but well-documented issue with COVID vaccines in young adults, particularly after 2nd or 3rd doses, and particularly in otherwise healthy males. There are issues related to the research on the relative frequencies of COVID/Vaccine myocarditis, but it does appear that younger men specifically may have a higher rate of vaccine myocarditis than COVID myocarditis.While the cases of vaccine myocarditis that do result in hospitalization largely appear to be self-limited and are associated with short hospital stays, long term follow up with cardiac MRIs demonstrates the persistence of scar in two-thirds of children who followed up. It is unknown at this time what the longer-term prognosis of this finding is.
Summary
- At this time, boosters do not durably protect individuals from infections, do not reduce transmission, expose individuals to the risk of vaccine associated myocarditis, and could even impair immunologic responses to future variants.
- Coercing patients to get a medical therapeutic in this context undermines trust in public health institutions and is unethical.
Anish Koka is a cardiologist (follow him on twitter @anish_koka). Viral Myalgia is a very smart doctor and data scientist (follow him on twitter @contrarian4data)
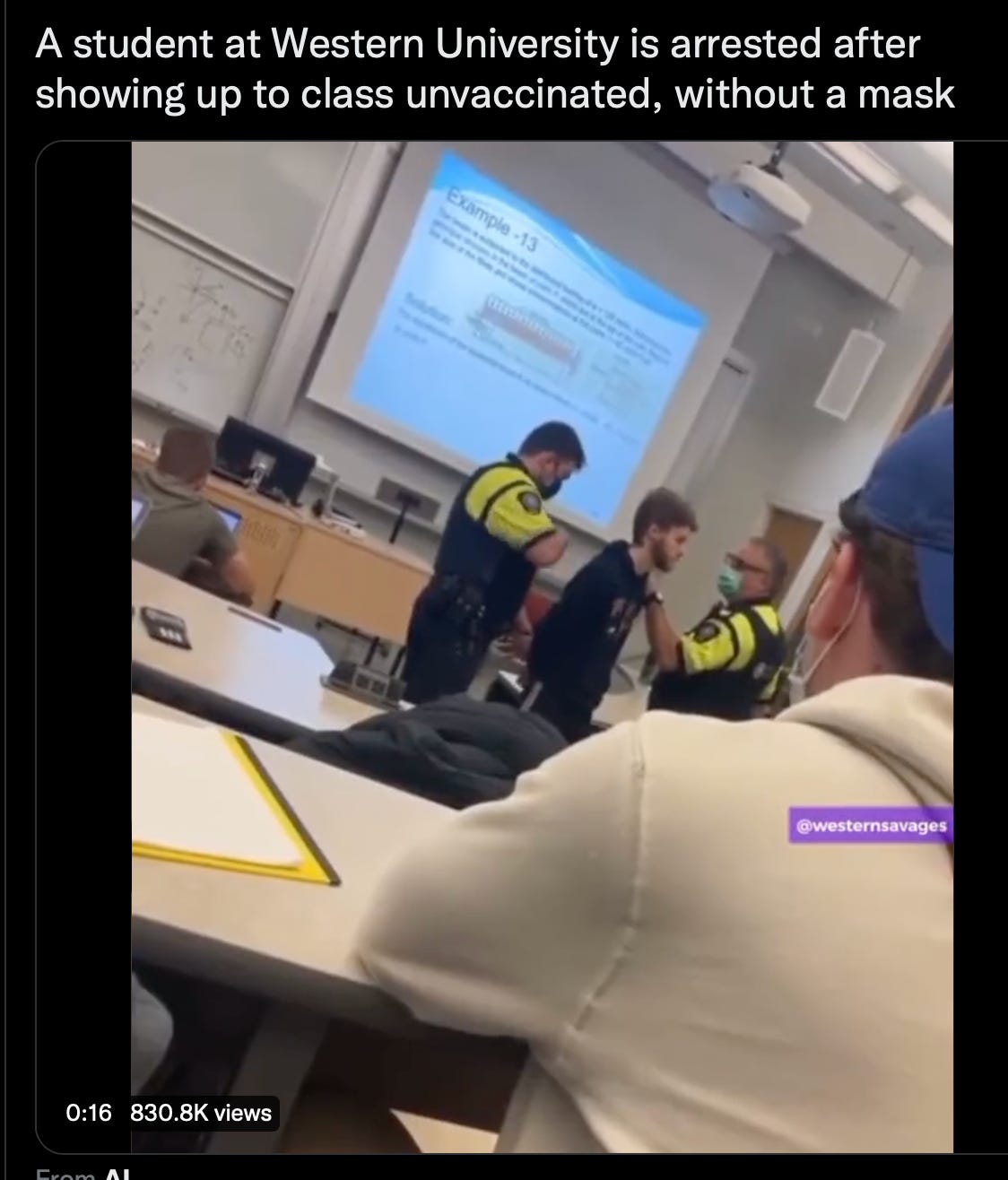
PS. Update at Western University.
PPS. I have to make the obligatory post-script here that I oversaw the administration of hundreds of mrna vaccines starting in March of 2021 in my cardiology clinic. The vaccine efficacy data for the original data was from thousands of patients and I certainly felt given the devastation wreaked on many of my patients in 2020 that the vaccines were the best chance of avoiding morbidity and mortality. The process to get the vaccines from the city department of health was a somewhat arduous 3-month process, and once the vaccines were on hand, there were daily reporting requirements that I dutifully performed for the many months we were administering vaccines. To accommodate the rush of patients, employees, volunteers, and conscripted children worked multiple weekends to administer the vaccines. So, I’m especially disgusted by medical colleagues and others who label any concerns registered about vaccine adverse events as “anti-vaxx”. Registering concern over a vaccine adverse event does not make doctors or patients “anti-vaxx”.
Anish Koka is a cardiologist (@anish_koka). Viral Myalgia is a very smart doctor and data scientist (@contrarian4data).
Categories: Uncategorized