
By KIM BELLARD
A relative — obviously overestimating my healthcare expertise — asked my thoughts on The New York Times article Can a Federally Funded ‘Netflix Model’ Fix the Broken Market for Antibiotics? I had previously skimmed the article and was vaguely aware of the Pasteur Act that it discusses, but, honestly, my immediate reaction to the article was, gosh, that may not be a great analogy: do people realize what a tough year Netflix has had?
I have to admit that I tend to stay away from writing about Big Pharma and prescription drugs, mainly because, in a US healthcare system that seems to pride itself on being opaque, frustrating, and yet outrageously expensive, the prescription drug industry takes the cake. It’s too much of a mess.
But a “Netflix model” for drug development? Consider me intrigued.
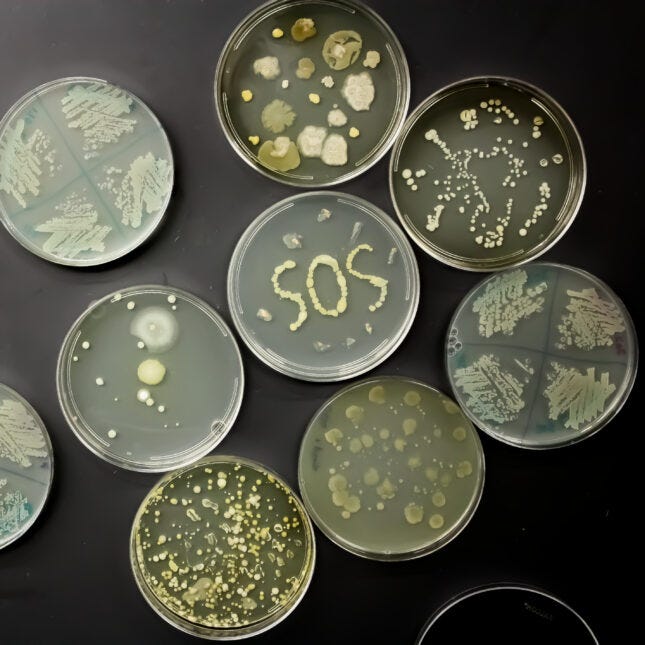
It’s easy to understand why market forces might not do well with rare diseases that need an “orphan drug,” but the “subscription model” approach that the Pasteur Act seeks to address is something that most of us need: antibiotics. Antibiotic resistance has made many of our front-line antibiotics less effective, but discovering new antibiotics is a slow, expensive process, and many pharmaceutical companies are reluctant to take the risk. The Pasteur Act would essentially pay for their development in return for “free” use of subsequently invented drugs.
There is widespread support for the bill (including, no surprise, PhRMA). Carlos del Rio, president of the Infectious Diseases Society of America (among other roles) writes: “PASTEUR is a unique financing model that creates a reliable market for critically needed antimicrobials — and as a result, promises to ignite a desperately needed revitalization in antimicrobial development.” That’s the hope.
It is worth noting that the U.K. has been testing such a model since 2020, but results so far are inconclusive. Glover, et. alia argue:
…the current subscription funding does not convincingly reward innovative research into new chemical space, a field that many small and medium-sized enterprises are struggling to attract funding for….Rather than supporting a resilient, innovative, commercial antibiotic ecosystem, there seems to be a marked risk that the UK subscription model could fall prey to what is termed the folly of rewarding A when hoping for B.
It wasn’t their intent, but I don’t think I’ve ever read a better description of the US healthcare system than “rewarding A when hoping for B.”
Critics of the Pasteur Act wrote a letter to Congress in November, warning: “Under the Pasteur Act, taxpayer dollars will be wasted as a blank check to pharmaceutical manufacturers for antimicrobials of limited benefit,” One of the signators of that letter, Reshma Ramachandran, argues in The Hill: “PASTEUR would instead signal to drug companies that they can continue the same lackluster antimicrobial development — paid for in large part by the public already — divorced from improving patients’ health.”
Let’s see: the existing business model has led to huge profits for Pharma, high prices for consumers, and yet not enough antibiotics or rare disease drugs, so, no, I’m not keen on subsidizing that industry with guaranteed, upfront payments.

The NYT article mentions other approaches that are being tried to incent antibiotic development. Carb-X (Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator) is a global partnership whose mission is: “Accelerate a diverse portfolio of innovative antibacterial products towards clinical development and regulatory approval with funding, expert support and cross-project initiatives.” It announced its latest funding rounds, targeted at three product categories, in October.
Another NYT article discussed development not of antibiotics but for rare diseases, mentioning n-Lorem, a non-profit foundation that “is focused on creating individual treatments for patients in the United States with nano-rare diseases caused by genetic mutations that affect approximately < 30 patients in the world.” It relies on donations, and has been surprisingly successful in its fundraising to-date, but, as the NYT notes: “Some rare disease experts are skeptical that one nonprofit organization will be able to serve every patient who needs help.”
Some researchers have proposed, instead of the Pasteur Act, setting up federally funded non-profits, staffed by microbiologists, medical chemists, and pharmacologists and overseen by a board of patient advocates, doctors, industry representatives, and others. Dr. Brad Spellberg, one of the authors of the proposal, told KHN: “They would not focus on one drug, per se. They would focus on discovering and developing new, impactful technologies.”
What I don’t want to see, and what I fear the Pasteur Act might do, is to lock in existing approaches with existing companies. As I’m fond of saying, it’s the 21st century; we need 21st century approaches. In particular, taking advantage of our microbiome and synthetic biology.
Just in the past few weeks, we’ve learned that the gut microbiome may drive our motivation to exercise, can be used to improve symptoms of autism and inflammatory bowel disease, and is connected to multiple sclerosis (MS) and depression, binge-eating, and heart-failure. We’re just scratching the surface of the impact of our microbiome on our health, but we know that all those antibiotics we’re keen on wreak havoc on it. Oh, and by-the-way, it is pretty good at developing antibiotics of its own.
We’ve been testing what I’ll call primitive efforts of using fecal transplants to boost the microbiome (the FDA just approved the first such treatment last month). Kate Macbride, writing in Inverse, says: “This approval is likely only the start of a promising future for prescription poop” (otherwise referred to as referred to as fecal-microbial therapy, or FMT).
Alison Halliday, PhD, goes a step further. In Technology Networks, she writes: “Scientists are harnessing the power of synthetic biology to develop a variety of medical applications — from powerful drug production platforms to advanced therapeutics and novel diagnostics.”
Jim Collins, Termeer professor of medical engineering and science at MIT, tell her: “By approaching biology as an engineering discipline, we are now beginning to create programmable medicines and diagnostic tools with the ability to sense and dynamically respond to information in our bodies.” He notes: “By applying synthetic biology, we have designed a living therapeutic that has the potential to help counter the potential negative effects of antibiotic use.”
Ms. Macbride points out: “Advances in synthetic biology are enabling researchers to create engineered probiotic bacteria that can sense, record and report on changes occurring inside the gut.” That’s some 21st century medicine.
So, don’t give me a “Netflix” for drugs that gives us reruns and spinoffs, from the same old companies that have been producing them. Give me one that looks ahead to new approaches (like synthetic biology), new theories of medicine/health (like microbiome-based).
Kim Bellard is a former payer exec, former editor at Tincture.io and now THCB regular
Categories: The Business of Health Care









