By GRACE CORDOVANO
Attending HLTH 2021 in-person in Boston solidified that there is no comparison between attending live vs. virtual conferences. While content and presentations can be solid both virtually or in-person, it is the energy of the connections that are made between scheduled presentations and the conversations that are shared throughout that move the needle. Kudos to the organizers of HLTH 2021 for prioritizing the safety of all in-person attendees with COVID-19 vaccination requirements, proof of negative PCR testing within 3 days of arrival, and mask requirements on-site.
After reflecting on all the proceedings, the conversations, and the experiences at HLTH 2021, here are eight reflections on the event from the patient and carepartner perspective.
1) Patients and Carepartners (Not) Included
These words were the taglines of HLTH2021:
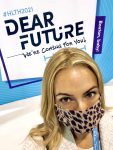
Dear Future: We’re coming for you. #HLTH2021
The largest and most important conference for health care innovation
A battle cry for improving health care, but I can’t help but wonder, who’s “we’re”?
The agenda and stages at HLTH2021 were filled with some of the biggest, most respected names in the health care ecosystem. Unfortunately, no patients were speaking from these stages. A search of the agenda and speaker list for “patient” showed entries for “patient experience” or “patient” in the form of an executive title. Many panels and discussions fell short of the real-world experiences of living life with a diagnosis or multiple comorbidities, the difficulties of barriers to healthier living that are caused by social determinants of health (SDoH), and disgraceful realities of the inefficiencies of workflows patients and their families face. There were no patient or carepartner champions sharing the positive impact that a company’s brand has had on their or their loved ones’ lives.
Continue reading…












