By SHUBHRA JAIN & JAY SANTORO


Knowledge is power. If this adage is true, then the currency of power in the modern world is data. If you look at the evolution of the consumer economy over the past 100 years, you will see a story of data infrastructure adoption, data generation, and then subsequent data monetization. This history is well told by Professors Minna Lami and Mika Pantzar in their paper on ‘The Data Economy’: “Current ‘data citizenship’ is a product of the Internet, social media, and digital devices and the data created in the digitalized life of consumers has become the prime source of economic value formation. The database is the factory of the future.” If we look no further than the so-called big tech companies and distill their business models down in a (likely overly) reductionist fashion: Apple and Microsoft provide infrastructure to get you online, and Facebook (Meta) and Google collect your data, while providing a service you like, and use that data to sell you stuff. Likely none of this is surprising to this audience, but what is surprising is that this playbook has taken so long to run its course in one of the world’s largest and most important sectors: healthcare.
Given the potential impact data access and enablement could have on transforming such a large piece of the economy, the magnitude of the opportunity here is — at face value — fascinating. That said, healthcare is a different beast from many other verticals. Serious questions arise as to whether target venture returns can be extracted in this burgeoning market with the scaled incumbents (both within and outside healthcare) circling the perimeter. Additionally, this is a fragmented ecosystem that has existed (in its infancy) for a few years now with well-funded players now solving for different use cases. Thus, another question emerges as to which areas are best suited for upstarts to capitalize. A key theme in our assessment of the space is that regulation is driving the move towards democratized data access in healthcare, but unlike in regulatory shake-ups of the past, this time start-ups will benefit more than scaled incumbents. Furthermore, we have identified some areas within each approach to this new ecosystem that particularly excite us for net new investment. Let’s dive in.
Why This Time is Different: Regulatory + Market Dynamics
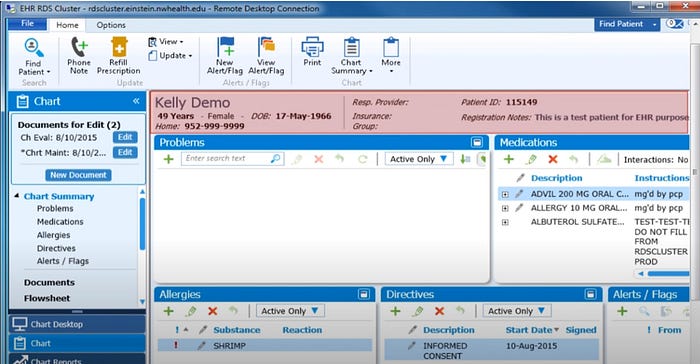
The Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009 brought about an explosion of digital healthcare data by expanding adoption of electronic medical records from ~12% to 96%.






 Paul Black is CEO of
Paul Black is CEO of  “We did not spend $35 Billion to create 5 data silos.” This was said by Vice President
“We did not spend $35 Billion to create 5 data silos.” This was said by Vice President 







