
By ALYA AHMAD, MD
Call it what you want, white privilege and health disparity appear to be two sides of the same coin. We used to consider ethnic or genetic variants as risk factors, prognostic to health conditions. However, the social determinants of health (SDOH) have increasingly become more relevant as causes of disease prevalence and complexity in health care.
As a pediatric hospitalist in the San Joaquin Valley region, I encounter these social determinants daily. They were particularly evident as I treated a 12-year old Hispanic boy who was admitted with a ruptured appendix and developed a complicated abscess, requiring an extensive hospitalization due to his complication. Why? Did he have the genetic propensity for this adverse outcome? Was it because he was non-compliant with his antibiotic regimen? No.
Rather, circumstances due to his social context presented major hurdles to his care. He had trouble getting to a hospital or clinic. He did not want to burden his parents—migrant workers with erratic long hours—further delaying his evaluation. And his Spanish-speaking mother never wondered why, despite surgery and drainage, he was not healing per the usual expectation.
When he was first hospitalized, his mother bounced around in silent desperation from their rural clinic to the emergency room more than 20 miles from their home and back to the clinic, only to be referred again to that same emergency room. By the time he was admitted 2 days later, he was profoundly ill. The surgeon had to be called in the middle of the night for an emergency open surgical appendectomy and drainage. Even after post-operative care, while he was on broad-spectrum intravenous antibiotics, his fevers, chills and pain persisted. To avoid worrying his mother, he continued to deny his symptoms. Five days after his operation, he required another procedure for complex abscess drainage.
In a 2007 study published in The New England Journal of Medicine, “We Can Do Better—Improving the Health of the American People,” Steven Schroeder describes the proportional contributors to premature death. Behavioral patterns & social circumstances dominate:
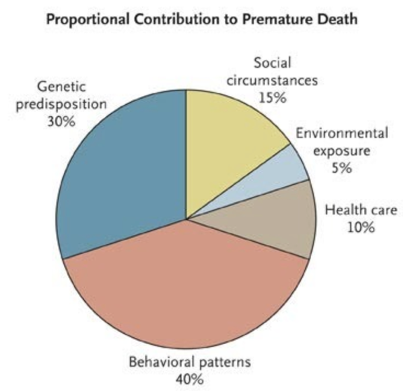
More recently, there appears to be a paradigm shift in how access to care and health care systems are viewed. As Schroeder demonstrated, health care delivery plays a relatively minor role in its impact on premature death. What governs the individual behavior of patients are the SDOH, which are a product of:
- Barriers to appropriate health care
- Economic instability
- Unsafe environment
- Poor health literacy and education
- Limited social and community support
- Food scarcity
- Social discrimination and language barriers
These are just a few of the factors that contribute to challenges in patient care and health inequities. Interestingly enough, genetics actually plays a relatively minimal risk factor for disease conditions & diagnosis. We cannot just say that Black people have a greater risk of heart disease, diabetes, hypertension, etc. We need to ascertain the social context of our diverse populations in order to address the incidences of chronic disease and its effects. The issue cannot simply be blamed on the genetics of the immigrant, the refugee, the homeless, or impoverished populations that lead to greater morbidity and mortality.
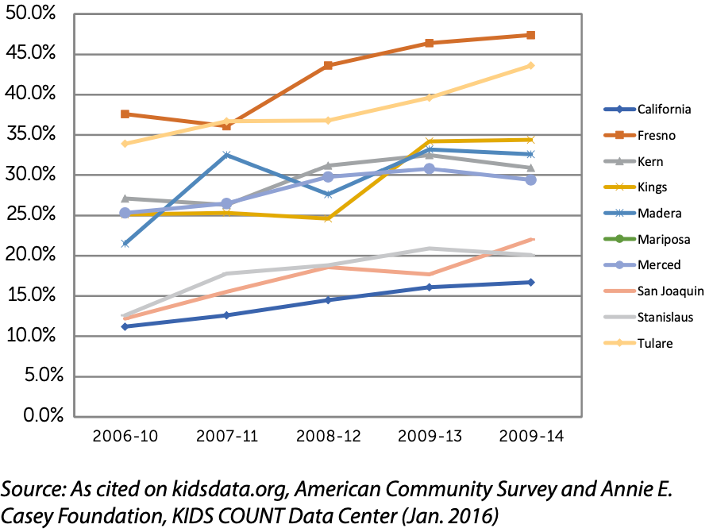
As a pediatrician practicing in the Central Valley, I see the consequence of social complexity in pediatric care delivery every day. In a recent 2017 report by the Center for Regional Change and Pan Valley Institute, California San Joaquin Valley, children in the area are “living under stress.” They are not only born under duress but face lifelong barriers to better physical and mental health. The occurrence of child poverty levels in counties of the San Joaquin Valley (SJV) are profound. The graph below shows poverty levels of 28% to 38% in the valley:

Additionally, California has a large Gross Domestic Product in terms of agriculture production in the country. When you break it down by county, crop value in the valley ranks high. Yet, the valley with the largest crop production also paradoxically has the highest child poverty in the state. Even with economic stability, poverty remains rampant in the central valley. The rates of concentrated poverty, where more than 30% of the population are below the Federal Poverty Level (FPL), are greatest in SJV areas and are increasing over time:
Percentage of children under 18 living in areas of concentrated poverty
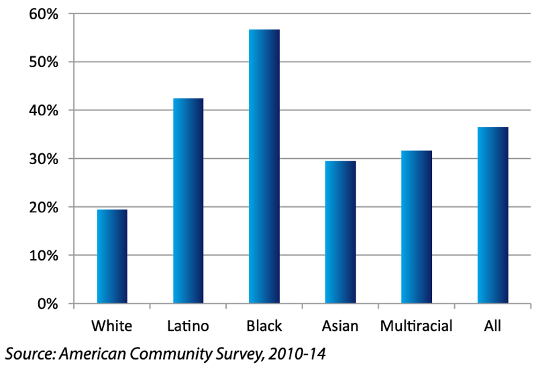
Furthermore, poverty rates are highest among children of color. The ethnic gap in poverty is 10-35%.
Percentage of San Joaquin Valley Children under 6 in Poverty, by Race/Ethnicity
Despite the economic potential, health care access and resources also operate at crisis levels. Rural communities with geographic obstacles face shortages in provider availability and health care systems. The same fertile communities of SJV, producing the food source of the nation, ironically have the largest limitations of access to food. Food scarcity, where food and especially healthy food is either limited or uncertain, remains above 26 to 29% when compared to a food shortage for the whole of California, which is at 23%.
Estimated Percentage of Children under 18 living in Households with Limited or Uncertain Access to Adequate Food, 2014

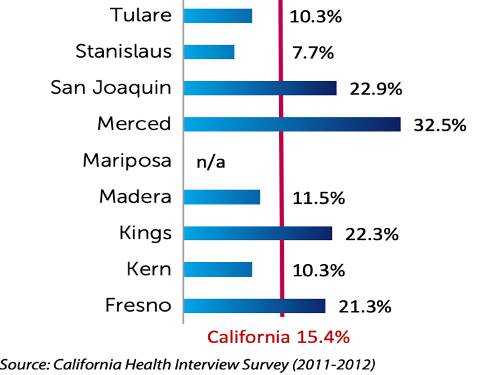
The overall pollution burden, which represents the potential exposures to pollutants and adverse environmental conditions caused by pollutants, is greater than 8 to 10% in the Valley. Not surprisingly, asthma and lung diseases in SJV districts are highest in central California.
Percentage of children diagnosed with asthma
Scientific literature now highlights Adverse Childhood Experience (ACE) in which the number of exposures of toxic stress and trauma: child abuse, neglect, domestic violence, parental drug/ alcohol exposure, incarceration, separation, and or stress, is scored. The greater number of ACE’s, the greater degree of maladaptive physiological, neuro-architectural, immunological, and epigenetic effects on the fetal and developing children. The effect of ACE’s on mental health and chronic medical conditions, (asthma, diabetes, cancer, heart disease, obesity, etc.) correlates exponentially with the number of ACE exposures. Such that, if a child has more than 4 ACE exposures, the risk of developing COPD (Chronic Obstructive Pulmonary disease) as an adult increased by 260%; for depression, it increased by 460%. In California, the prevalence of the number of ACEs with 2 or more toxic level stress exposures early in the child’s life is at 16.7%. Per kidsdata.org, a Population Reference Bureau, analysis of data from the National Survey of Children’s Health and the American Community Survey (Mar. 2018) the incidence of parent-reported ACE scores >2 for the SJV counties is even higher: Fresno, Tulare, Madera, and Merced cities range from 17.9 to 19.3% of the population. Such that 1 out of 5 children are exposed to toxic level stress. The consequences of that same child becoming an adult with a chronic medical and or mental condition cannot be discounted.
Health vulnerabilities in the valley are extreme and burden the limited health care systems servicing the community in SJV. The current California governor’s administration has acknowledged this fact. Support to implement and maintain medical education and training programs with retention of providers in SJV is necessary. Specific funding allotments for improving mental health, air quality, homelessness among many other SDoH’s in the region is vital.
Dr. Nadine Burke-Harris, California’s first female Surgeon General, who recently visited the Valley, announced an ACEs Aware campaign. The ACEs Aware initiative is a first-in-the-nation statewide effort to screen for childhood trauma and treats the impact of toxic stress. The bold goal of this state-wide initiative is to reduce Adverse Childhood Experiences and toxic stress by half in a single generation . and to launch a national movement to ensure everyone is ACEs Aware. ACEs Aware is not only a complete program with training and readily available tools to implement screening, it is also a fully reimbursed program in a preventative pediatric care setting.
Starting early, as pediatricians, we can identify kids exposed to ACEs through routine screenings and establish prevention programs in health care, schools and youth-serving organizations. In their critical and early developmental stages, resource allocation of health services can be provided. It is also imperative to know and stay engaged with our region’s leaders, telling our stories in health care, enlist our community partners, schools, regulatory agencies, and empower our patients and families to advocate for social and health equity.
Alya Ahmad MD FAAP is a pediatric hospitalist who has worked in both private and academic centers as a professor and faculty and blogs at The Context of Care.
Categories: Uncategorized









