Will ACO (accountable care organization) IT models be walled gardens or open platforms? i.e., will ACO IT platforms focus on exchanging information within the provider network of the ACO, or will they also be able to exchange information with providers outside the ACO network? (If the question still isn’t clear, click here for a further explanation.).
One POV: ACO’s Will Need Open IT Platforms
Mike Cummens, M.D., associate chief medical information officer at 750-physician Marshfield Clinic in Wisconsin, is quoted in a recent article in Healthcare Informatics . Dr. Cummens argues for an open ACO IT approach:
. Dr. Cummens argues for an open ACO IT approach:
There will be an emphasis on transfer-of-care summaries and how to facilitate information sharing across the full continuum of care, he said. “For instance, you will have to work into care management plans the notification of home health agencies,” Cummens added. “In an ACO model, you will have to have methods in place to communicate all this information to providers who are not part of your own organization. People will have an option to see providers outside an ACO, so you will need to be able to transfer care summaries and discharge summaries outside the ACO.”
Also, because patient involvement is a key part of ACOs, the IT infrastructure will have to support patients signing off on their care plans and document their progress toward reaching goals, he noted. That will involve some type of self-management tools and personal health record access to their own data.
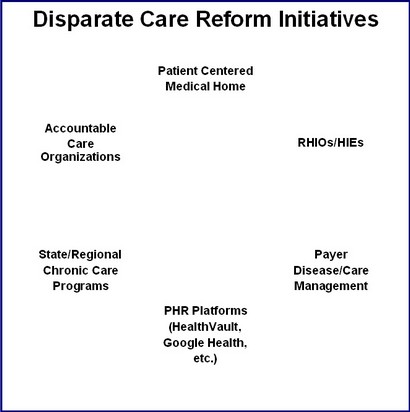
Cummens noted that the patient-centered medical home is geared toward an individual practice, and meaningful use metrics are geared toward providers, but ACOs will require managing data across enterprises. “When we visualize this and realize we are dealing with multiple electronic health records, the infrastructure for ACOs really has to ride on top of that,” he said. He sees the need for a new type of system, probably outside the EHR, that can bridge organizations, allow for risk assessment and analytics and reach down into tools for day-to-day management. That’s a tall order.