BY MICHAEL MILLENSON
In 1767, as American colonists’ protestations against “taxation without representation” intensified, a Boston publisher reprinted a book by a British doctor seemingly tailor-made for the growing spirit of independence.
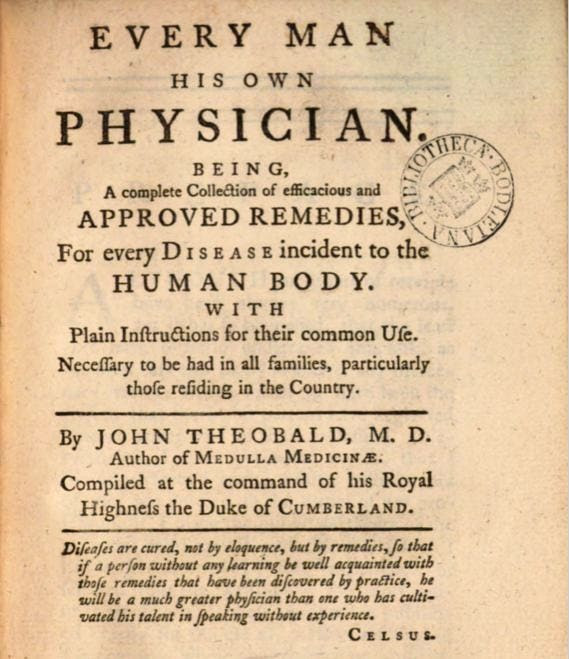
Talk about “democratization of health care information,” “participatory medicine” and “health citizens”! Every Man His Own Physician, by Dr. John Theobald, bore an impressive subtitle: Being a complete collection of efficacious and approved remedies for every disease incident to the human body. With plain instructions for their common use. Necessary to be had in all families, particularly those residing in the country.
Theobald’s fellow physicians no doubt winced at the quotation from the 2nd-century Greek philosopher Celsus featured prominently on the book’s cover page.
“Diseases are cured, not by eloquence,” the quote read, “but by remedies, so that if a person without any learning be well acquainted with those remedies that have been discovered by practice, he will be a much greater physician than one who has cultivated his talent in speaking without experience.”
Translation: You’re better off reading my book than consulting inferior doctors.
To celebrate Americans’ independent spirit, I decided to compare a few of Dr. Theobald’s recommendations to those of his 21st-century equivalent, “Dr. Google.” Like Dr. Google, which receives a mind-boggling 70,000 health care search queries every minute, Dr. Theobald also provides citations for his advice which, he assures readers, is based on “the writings of the most eminent physicians.”
At times, the two advice-givers sync across the centuries. “Colds may be cured by lying much in bed, by drinking plentifully of warm sack whey, with a few drops of spirits of hartshorn in it,” writes Dr. Theobald, citing a “Dr. Cheyne.” Dr. Google’s expert, the Mayo Clinic Staff, proffers much the same prescription: Stay hydrated, perhaps using warm lemon water with honey in it, and try to rest. Personally, I think “sack whey” – sherry plus weak milk and sugar – sounds like more fun.
Continue reading…











